Assessment and care planning go hand in hand. Assessment is the process in which we determine what the client’s needs, strengths, goals, and limitations are. Care planning is the process in which we determine how to address those needs, strengths, goals, and limitations. Just like assessment, care planning is an ongoing process. At the onset of treatment, a full clinical assessment is completed and an initial set of clinical recommendations are provided. As the client moves through treatment, providers continuously re-assess and re-strategize, adjusting to the client’s progress and documenting their conclusions in progress notes.
Prior to July 2022, DHCS required that all services provided be present on a formal treatment plan before being provided. This made adjusting to a client’s changing situation and needs difficult, as providers were not allowed to be flexible in the services they provided. With the CalAIM documentation changes that went into effect in July 2022, the requirement for a formal treatment plan went away for most behavioral health services. Now, instead of creating a formal treatment plan, behavioral health providers can simply provide informal care planning, which is meant to be “an ongoing, interactive component of service delivery rather than a one-time event.” (BHIN 23-068, page 11) This allows for the needed flexibility to meet the ever changing needs of our clients.
Now, providers can simply document their care plan for a client in their progress note using everyday language. This includes documenting the types of services you plan to provide and any plans to coordinate with other providers. This can include a client’s desires and goals for treatment in their own words, as well as any strengths or resources that can help them achieve this. It’s not a formalized list, but rather a clinical summary of recommendations provided at an ongoing, organic tempo, that changes alongside the client.
For most services, this is plenty to document that care planning is occurring. Some services, programs, or facilities still have specific requirements to include in any care planning done. BHIN 23-068, Enclosure 1a, provides a list of these programs, services, or facilities, as well as the regulations and guidance that governs them. Even still, most of these regulations don’t require a formal treatment plan, instead simply listing a requirement to include specific elements, that the plan for care must be reviewed regularly, that the client/guardian be involved with the creation of the plan, or that the plan be signed by a provider. All of these requirements can still be met within the progress note.
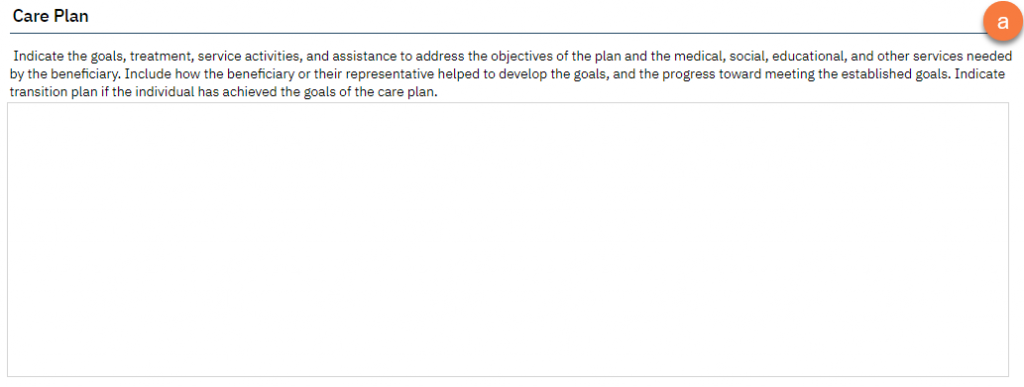
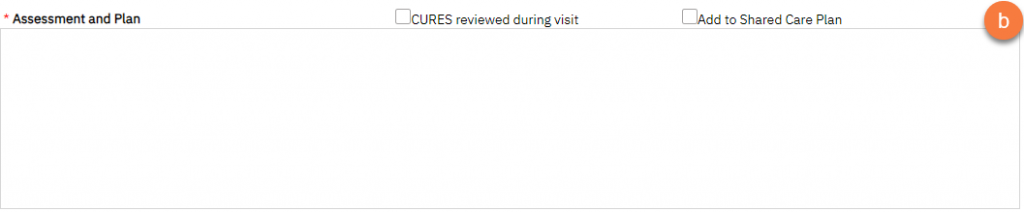
In SmartCare, there are 2 main service notes that are used as progress notes. Both of these have a field for documenting the plan of care. In the Progress Note, this is the “Care Plan” field.(a) In the Psych/Med Note, this is the “Assessment and Plan” field.(b)
These sections are “pulled forward” to subsequent notes of the same type within the same program. For progress notes, this will pull forward regardless of provider. For the Psych/Med Note it will only pull forward for the same provider.
- Jennifer, an LCSW, completes an Assessment in the Adult Behavioral Health Clinic program for Humphrey, a 27-year-old client, and then writes a service note using the Progress Note template. She documents her initial recommendations for Humphrey’s treatment in the “Care Plan” field. She signs the note.
- Maulik, a Certified Peer Specialist, begins working with Humphrey in the Adult Behavioral Health Clinic program as well. When he creates his first service note for Humphrey, the “Care Plan” field on the Progress Note includes what Jennifer wrote in her most recent note. (same note type, same program)
- Dan, an MD, begins working with Humphrey in the Adult Behavioral Health Clinic program. When writing his service notes, he uses the Psych/Med Note template. Since this is a different note type than the Progress Note, the “Assessment and Plan” field is blank. (different note type, same program)
- Jennifer then refers Humphrey to a new program, the Peer-Led Groups program. Justin begins to work with Humphrey through the Peer-Led Groups program. When he writes his first service note, which uses the Progress Note, the “Care Plan” section is blank, since this is a new program. (same note type, different program)
This means that the plan of care is an active, living document that includes interventions from all members of the treatment team within a given program. For small programs, this may only include one or two providers. Some larger programs may wish to clarify treatment team roles and responsibilities by associating treatment team members with specific interventions. When a specific type of provider must sign the plan of care, this is addressed by them signing their service note.
Since the care plan lives in the client’s service notes, the plan of care is reviewed every time a service note is completed. Changes to the care plan can and should be made as the client’s needs change. This allows for quick and reliable communication between treatment team members, as they will also see any updates to the care plan just by writing their own service note. This addresses any requirement to review and/or update the plan of care at regular intervals.
Documenting a client or guardian’s participation and agreement does not necessarily require a signature by that person. Documenting conversations with the client/guardian about their treatment easily demonstrates their participation in the creation and their agreement of the plan of care. Including direct quotes can also add a nice touch, especially for documenting the client’s own personal goals for treatment.
Just make sure that you know the documentation and treatment requirements for your program and abide by those requirements.
Requirements for the Client/Guardian to Sign a Treatment Plan
Some programs, services, or facilities require a client or guardian to sign a treatment plan. This can be done by having the client sign the service note, but these facilities often have additional, more strict requirements that necessitate a more formal treatment plan. For those services that require the client/guardian to sign a treatment plan, clinicians should use the Interdisciplinary Treatment Plan. Again, make sure that you know the documentation and treatment requirements for your program and abide by those requirements.
See How to Complete the Interdisciplinary Treatment Plan for more information.
See Also:
Care Plan Requirements Per BHIN 23-068
| Program; Service; or Facility Type | Authority/ Background | Documentation Location |
|---|---|---|
| Children’s Crisis Residential Programs (CCRP) | Children’s Crisis Residential Mental Health Program Interim Standards | Interdisciplinary Treatment Plan |
| Community Treatment Facilities (CTF) | 9 CCR § 1927 subds. (a)(6) and (e) | Service Note |
| DMC-ODS Residential Treatment Services and Withdrawal Management Services provided in DHCS LOC designated AOD Treatment Facilities | BHIN 21-001 and attachments | Service Note |
| Enhanced Care Management (ECM) | ECM Policy Guide | Service Note |
| Mental Health Rehabilitation Centers (MHRC) | 9 CCR § 786.15 subds. (a); (d); (e) | Interdisciplinary Treatment Plan |
| Mental Health Services Act Full-Service Partnership (FSP) Individual Services and Supports Plan (ISSP) | 9 CCR § 3620 | Service Note |
| Peer Support Services | CMS Directors’ Letter 07-011; California State Plan Section 3 Att. 3.1-A Supp. 3; California State Plan Section 3 Att. 3.1-B Supps. 2-3 | Service Note |
| Short-Term Residential Therapeutic Programs (STRTPs) | Interim STRTP Regulations Version II Section 10 | Service Note |
| Social Rehabilitation Programs (SRPs). Includes programs certified by DHCS for: Short-Term Crisis Residential Treatment; Transitional Residential Treatment; and Long Term Residential Treatment | 9 CCR § 532.2 subds. (c) and (d) | Service Note |
| Substance Abuse Block Grant (SABG) Programs/Services | 45 CFR § 96.136(d)(3) | Service Note |
| Targeted Case Management (TCM); Intensive Care Coordination (ICC) | 42 CFR § 440.169(d)(2) | Service Note |
| Therapeutic Behavioral Services (TBS) | DMH IN 08-38; Emily Q. v. Bonta Nine-Point Plan (Appendix D) | Service Note |
Updated 8/6/2024
